Your Read is on the Way
Every Story Matters
Every Story Matters
The Hydropower Boom in Africa: A Green Energy Revolution Africa is tapping into its immense hydropower potential, ushering in an era of renewable energy. With monumental projects like Ethiopia’s Grand Ethiopian Renaissance Dam (GERD) and the Inga Dams in the Democratic Republic of Congo, the continent is gearing up to address its energy demands sustainably while driving economic growth.
Northern Kenya is a region rich in resources, cultural diversity, and strategic trade potential, yet it remains underutilized in the national development agenda.

Can AI Help cure HIV AIDS in 2025

Why Ruiru is Almost Dominating Thika in 2025

Mathare Exposed! Discover Mathare-Nairobi through an immersive ground and aerial Tour- HD

Bullet Bras Evolution || Where did Bullet Bras go to?
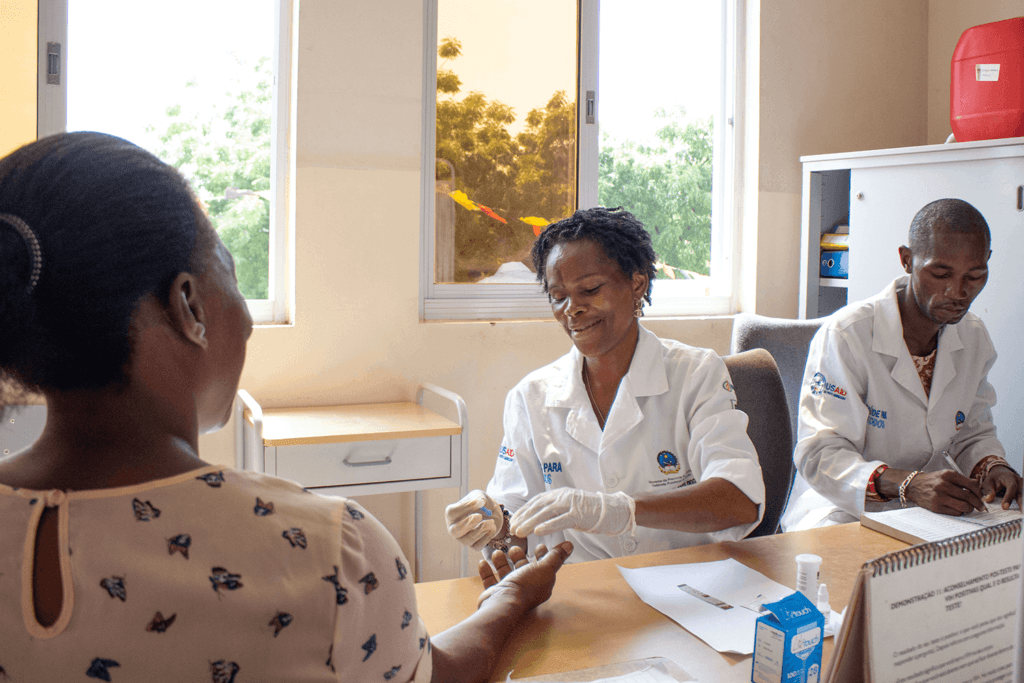
For decades, Kenya’s healthcare system has relied on generous donations from international organizations and foreign governments. These funds have played a crucial role in financing essential programs, particularly in the fight against HIV/AIDS, tuberculosis, and malaria. However, when a major foreign donor abruptly cut funding, the nation was thrown into a healthcare crisis of unprecedented scale. The Ministry of Health, already grappling with budgetary constraints, found itself scrambling to fill a Ksh.30 billion shortfall—a sum that seemed nearly impossible to raise through domestic means alone.
The funding freeze, which came as part of sweeping global policy changes, left Kenya’s healthcare sector exposed, highlighting just how dependent the country had become on external assistance. The sudden loss of financial support disrupted long-running programs, affecting not only the availability of life-saving medication but also the stability of health institutions that had come to rely on these funds. In particular, HIV treatment and prevention efforts faced a major setback, with the risk of treatment interruptions looming for thousands of patients. The question now facing Kenya was whether the government could step up and sustain these programs independently—or if the country would be forced to seek alternative international support.
In the wake of the crisis, the government was confronted with an urgent decision—where would the money to fill this funding gap come from? One of the most controversial proposals was to reallocate funds from infrastructure projects to healthcare. Some government officials argued that resources meant for road construction and other development projects could be diverted to sustain essential health services. Proponents of this move insisted that while roads and infrastructure are important for economic growth, nothing is more critical than a functioning healthcare system that directly saves lives.
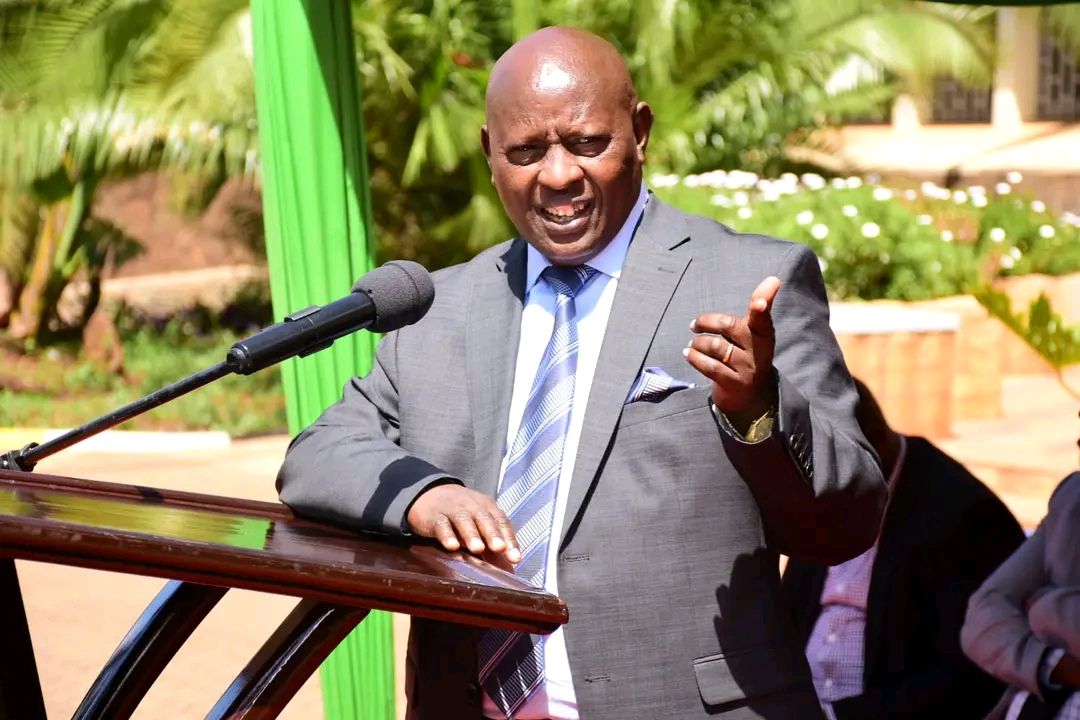
However, the proposal was met with fierce resistance from politicians who feared the political consequences of such a move. Infrastructure projects, particularly road construction, have long been used as a key political tool to gain voter support. Diverting funds away from these projects risked alienating constituents who equate visible development with government effectiveness. Nyeri Governor Mutahi Kahiga voiced the ethical dilemma at play: "We know roads win votes, but hospitals save lives." This debate underscored a deeper issue—Kenya’s financial priorities had long been skewed, with health often taking a backseat to other sectors. Now, with no external funding to fall back on, the nation was being forced to confront its spending habits and make tough choices.
Beyond funding reallocations, the impact of the aid freeze was already being felt across the country. Without sufficient funds, healthcare facilities began to experience shortages of essential medical supplies, including antiretroviral drugs (ARVs), tuberculosis medication, and malaria treatments. The supply chains that had been kept running by donor funding were now on the brink of collapse, putting thousands of patients at risk of treatment interruptions.
Additionally, thousands of healthcare workers who had been employed through donor-funded programs faced an uncertain future. Many of these professionals, including nurses, community health workers, and specialists in HIV treatment and prevention, were suddenly at risk of losing their jobs. These workers had been crucial in running Kenya’s HIV response efforts, offering testing, treatment, and counseling services to millions across the country. Their potential dismissal threatened to reverse years of progress made in managing HIV, TB, and other infectious diseases.
The situation was dire. Some clinics had already started turning patients away due to a lack of medication, and reports emerged of people being forced to travel long distances in search of treatment. If the crisis was not addressed swiftly, experts warned that Kenya could see a resurgence of preventable diseases, undoing decades of progress in public health. The country faced a stark reality—it either had to find a way to sustain these programs locally or watch as millions suffered due to inadequate care.

With foreign aid no longer a guaranteed lifeline, policymakers began to explore alternatives to keep the healthcare system running. One of the most widely discussed solutions was the need to develop Kenya’s local pharmaceutical industry. If the country could manufacture its own medical supplies rather than relying on expensive imports or donor-funded shipments, it could significantly reduce costs and ensure a more stable supply of essential drugs. However, this approach required substantial investment in research, production facilities, and regulatory frameworks—something the government had not previously prioritized.
Additionally, discussions emerged around restructuring the existing healthcare workforce. With thousands of donor-funded healthcare workers at risk of losing their jobs, officials debated whether these workers could be absorbed into the mainstream public healthcare system. The challenge, however, was that Kenya’s public health sector was already facing financial strain, and integrating these workers without additional funding would only stretch the system further.
Another proposed solution involved integrating HIV, TB, and malaria care into Kenya’s Social Health Authority (SHA) benefits package. This would ensure that these services were covered under the national health insurance system, making them more sustainable in the long run. However, the SHA itself was facing credibility issues, with many questioning its efficiency. Makueni Governor Mutula Kilonzo voiced these concerns bluntly: “If SHA doesn’t work, we need an exit strategy—not empty speeches.” This remark highlighted the frustration among stakeholders, who felt that existing systems were failing to address the urgency of the crisis.
As the crisis unfolded, one of the most glaring issues was the absence of Kenya’s National Treasury from key discussions. The government institution responsible for financial planning and budget allocation failed to show up at crucial meetings, further fueling frustrations. With no clear strategy in place, healthcare officials were left to fend for themselves, scrambling to find immediate solutions while also trying to formulate a long-term plan.
This moment represented a turning point for Kenya’s healthcare system. Would the government take decisive action to secure domestic funding and create a self-sustaining healthcare model? Or would it continue to rely on unpredictable foreign aid, leaving the country vulnerable to future funding cuts?
The road ahead would not be easy. Kenya needed not only financial resources but also strong political will to prioritize healthcare above other competing interests. If the country could learn from this crisis and implement sustainable solutions, it could emerge stronger and more self-reliant. However, if the government failed to act, the consequences would be severe—millions of Kenyans would be left without access to critical healthcare services, and years of progress in fighting infectious diseases could be undone.
In the coming months, Kenya’s ability to navigate this crisis would define its future. Would the country rise to the challenge, or would it fall back into a cycle of dependency? The answer would determine the health and well-being of generations to come.
0 comments